As we progress into 2025, the use of local anesthetic continues to be a cornerstone in medical and dental procedures, offering patients the advantage of pain-free interventions without the systemic effects associated with general anesthesia. Local anesthetic plays a crucial role in enhancing patient comfort and safety during various procedures, ranging from minor surgeries to dental work. Its ability to numb a specific area allows practitioners to perform intricate tasks while minimizing discomfort, significantly improving the overall patient experience.
However, alongside its numerous benefits, the use of local anesthetic is not without risks. Adverse reactions, while rare, can occur, including infections, allergic responses, or complications from improper administration. Understanding both the advantages and potential drawbacks of local anesthetic is essential for practitioners and patients alike. This guide delves into the top benefits and risks associated with local anesthetic, aiming to provide a comprehensive overview that empowers stakeholders to make informed decisions in the realm of healthcare.

Local anesthetics are a cornerstone in modern medicine, providing pain relief during various medical and dental procedures. Understanding their mechanism of action is crucial; these agents work by blocking sodium channels in nerve cells, inhibiting the transmission of pain signals to the brain. This allows patients to undergo procedures with minimal discomfort, enhancing overall experiences in both outpatient and inpatient settings.
The administration of local anesthetics can take various forms, including injections, topical applications, or nerve blocks. Each method is tailored to specific procedures or types of pain. While these substances are generally safe and effective, it is vital for practitioners to be aware of potential risks, such as allergic reactions or systemic toxicity, especially in high doses. The growing popularity of local anesthetics in diverse medical fields highlights the importance of understanding both their benefits and potential side effects as we move into 2025 and beyond. This awareness ensures that healthcare professionals can make informed decisions, optimizing patient care while minimizing complications.

Local anesthetics play a crucial role in pain management, offering several key benefits that are increasingly recognized in clinical practice as we look toward 2025. One significant advantage of local anesthetics is their ability to provide targeted pain relief with reduced systemic effects. According to a report from the American Society of Anesthesiologists, local anesthetics allow for effective analgesia in specific regions of the body, minimizing the need for general anesthesia in many procedures. This targeted approach not only enhances patient safety but also contributes to quicker recovery times, which is vital for popularity in outpatient settings.
Another notable benefit of local anesthetics is their versatility and effectiveness in various medical fields, from dentistry to orthopedic surgery. The Journal of Pain Research highlighted that an increasing number of proceduralists are incorporating local anesthesia into their practices due to its ability to improve patient comfort while also optimizing outcomes. Additionally, the growing use of regional nerve blocks has been associated with lower opioid consumption post-surgery, reflecting a broader trend towards minimizing reliance on opioids in pain management. As more healthcare providers adopt these techniques, the data indicates a shift toward sustainable pain management solutions that could reshape practices in the coming years.
Local anesthesia is widely recognized for its effectiveness in minimizing pain during medical procedures, but it is essential to be aware of the potential risks and side effects that can arise from its use. One of the most common side effects is localized swelling and tenderness at the injection site, which, while typically temporary, can be uncomfortable for patients. In some cases, patients might experience prolonged numbness or tingling, which can raise concerns about nerve damage, especially if the anesthesia is administered improperly.
More serious risks associated with local anesthesia include allergic reactions. Although rare, some individuals may develop hypersensitivity to the anesthetic agents.
Symptoms can range from mild skin reactions to severe anaphylaxis, necessitating immediate medical intervention.
There is also the possibility of systemic toxicity if anesthesia is inadvertently injected into a blood vessel, potentially leading to complications such as seizures or cardiovascular issues.
Awareness and proper administration techniques are critical in mitigating these risks to ensure patient safety during procedures involving local anesthesia.
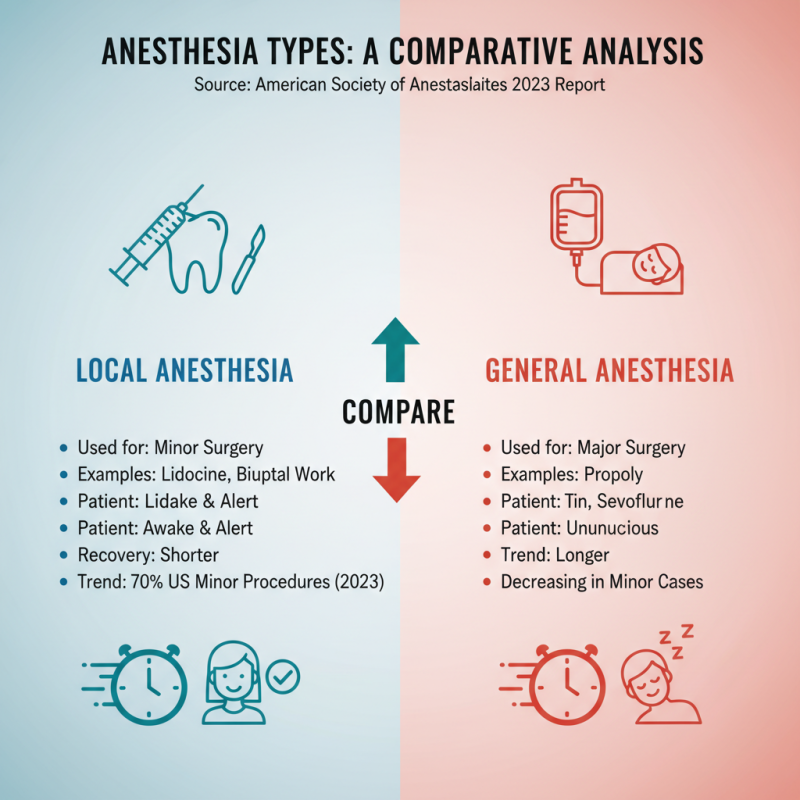
Local anesthetics and general anesthetics serve distinct roles in medical settings, each with its advantages and drawbacks. A comparative analysis illustrates that local anesthetics, such as lidocaine and bupivacaine, are typically used for minor surgical procedures and dental work, allowing patients to remain awake and alert. According to a 2023 report from the American Society of Anesthesiologists, the use of local anesthetics has increased in outpatient settings due to their efficacy in pain management and shorter recovery times. Statistics show that over 70% of minor surgical procedures in the U.S. now utilize local anesthesia, reflecting a growing trend toward more conservative, patient-friendly approaches.
In contrast, general anesthesia involves rendering patients completely unconscious, often required for more invasive surgeries. Although it provides a deeper level of sedation, the risks associated with general anesthesia can be higher. Data from the World Health Organization indicates that adverse events occur in roughly 5-20% of patients undergoing general anesthesia, greater than the <1% risk linked to local anesthetic procedures. Furthermore, the side effects of general anesthetics can include prolonged sedation and post-operative nausea, which contribute to longer recovery periods. As surgical techniques continue to evolve, the choice between local and general anesthesia increasingly hinges on the specific procedural requirements and patient health profiles, making informed discussions between healthcare providers and patients essential.
As we move into 2025, the landscape of local anesthetic use is evolving rapidly, driven by advancements in medical technology and a deeper understanding of patient safety protocols. One notable trend is the development of longer-lasting and more effective formulations that minimize discomfort and enhance recovery times. Healthcare providers are increasingly adopting multimodal analgesia approaches, combining local anesthetics with other medications to optimize pain control while reducing reliance on systemic opioids. This holistic view of pain management not only improves patient satisfaction but also aligns with contemporary safety initiatives aimed at reducing side effects and potential complications.
For patients considering procedures involving local anesthetics, it's essential to be proactive about safety. Here are a few quick tips: